Aim: Determination of TDP & TDT of E.coli for designing of a sterilizer.
BACKGROUND
One of the most popular and traditional methods of germ control is heating. It is utilized in straightforward processes like canning and frying. By changing microbial membranes and denaturing proteins, heat can kill microorganisms.
The lowest temperature at which all microorganisms perish in a 10-minute exposure is known as a microorganism’s thermal death point (TDP). Some microbes (such endospore-formers like C. botulinum) are more heat tolerant than others when it comes to how they react to high temperatures. The duration of time is a comparable quantity known as the thermal death time (TDT).
Needed at a specific temperature to completely destroy all germs in a sample. When describing sterilizing processes that make use of high heat, such autoclaving, these characteristics are frequently employed.
One of the earliest forms of wet heat is boiling. control of microorganisms, and certain viruses and vegetative cells are normally killed with reasonable efficiency. Boiling, however, does not completely destroy endospores; some endospores can withstand boiling for up to 20 hours.
Furthermore, since boiling takes longer to destroy microorganisms at higher altitudes due to the lower boiling point of water, boiling may be less effective there. Due to these factors, boiling is not regarded as a reliable sterilization method in a clinical or laboratory setting.
In the laboratory or clinic, a wide variety of heating protocols can be employed for sterilization. These protocols can be divided into two primary groups: moist-heat sterilization and dry-heat sterilization. Sterilizing inoculating loops is one example of an aseptic approach that uses direct application of high heat during dry-heat sterilization in the laboratory.
All microbes are destroyed by incinerating at extremely high temperatures. A dry-heat sterilizer, such as an oven, can also be used to apply dry heat for relatively lengthy periods of time (at least two hours) at temperatures as high as 170 °C. However, because moist heat penetrates cells more effectively than dry heat, moist heat sterilization is often the most successful method.
Autoclaves normally operate at pressures of 15 to 20 pounds per square inch and temperatures of 121 °C or, in certain situations, 132 °C (psi). Depending on the volume and type of material being sterilized, the exposure period will vary, but it will usually be 20 minutes or greater.
Larger volumes will require longer exposure duration to provide enough heat transfer to the items being sterilized. Instruments are wrapped loosely in paper or foil and containers are left partially closed because the steam must come into direct contact with the liquids or dry items that need to be sterilized. To completely sterilize items using an autoclave (sterilizer), the temperature needs to be high enough to kill endospores.
Quality control is crucial since sterilization is crucial to safe medical and laboratory practices. Recorders for keeping track of the pressures and temperatures reached during each run may be included in autoclaves (sterilizers). Along with the items to be sterilized, internal indicators of various kinds should also be autoclaved to make sure the correct sterilization temperature has been attained.
The use of heat-sensitive autoclave tape, which has white stripes that turn black when the proper temperature is reached after a successful autoclave run, is one frequent method of indication.
REQUIREMENTS
| S. no. | |
|---|---|
| 1 | E. coli culture |
| 2 | Luria-Bertani medium |
| 3 | Petri plates |
| 4 | Autoclave |
| 5 | Test tubes |
PROCEDURE
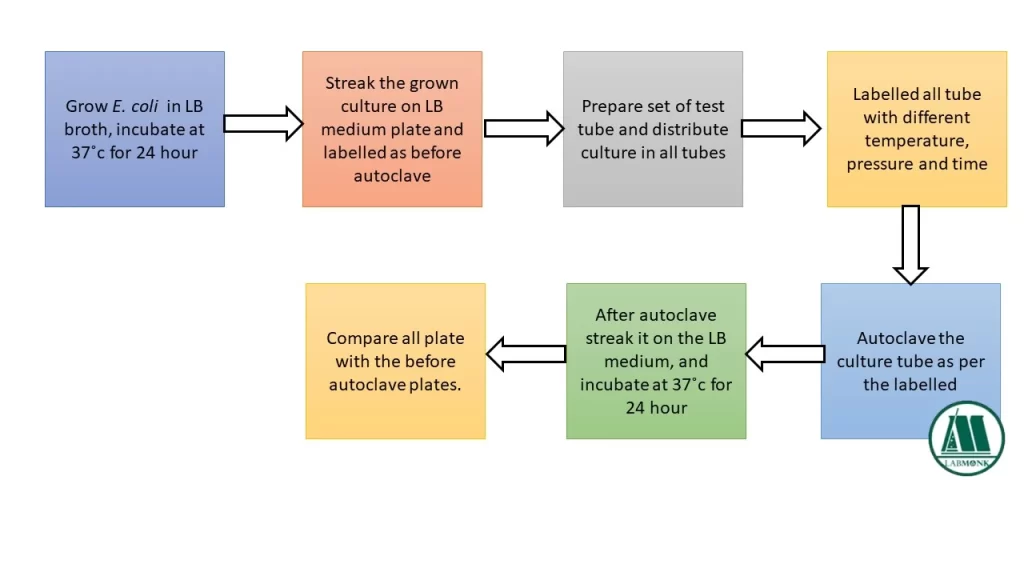
- Grow E. coli in 100 ml LB broth medium at 37˚c for 24 hours. [2]
- Streak the E. coli on LB medium plate, labelled it as before autoclave and incubate at 37˚c for 24 hours. [1]
- Prepare set of test tube labelled as different temperature, pressure and time for autoclave, and distribute grown E. coli culture to each tube.
- Autoclave the culture tubes at different temperature (110˚c, 121˚c, 132˚c), pressure (10 psi, 15 psi, 20 psi, 30 psi) and time (5 min, 10 min, 15 min and 30 min). [1]
- After the culture has been autoclave, streak it on the LB medium, labelled the plate same as culture tube and incubate at 37˚c for 24 hours.
- Observe for the growth of organism with before autoclave plate.
CONCLUSION
The study concludes that the thermal death point and thermal death temperature of E. coli for sterilizer design.
Also read:
- Effect of inhibitors on enzyme activity
- Methods for purification of enzymes
- Isolation of O & H Antigen from Salmonella typhi
- Microbial Staining Methods
- Microplate based Alamar Blue Assays
- Isolation of Genomic DNA from E. coli
- Estimation of DNA and its purity check using UV spectrophotometer (A260 measurement)
- Isolation of O & H Antigen from Salmonella typhi
- Screening for citric acid producing organisms
REFERENCES
- Joan Petersen and Susan McLaughlin, “Laboratory exercise in microbiology: discovering the unseen world through hands on investigation”, CUNY Academic Works, 2016.
- Shigenobu Mitsuzawa, Shigeru Deguchi and Koki Horikoshi, “Cell structure degradation in Escherichia coli and Thermococcus sp. Strain Tc-1-95 associated with thermal death resulting from brief heat treatment”, Federation of European microbiological Societies, 2006.
- https://nevsink.com/temperature-and-time-requ-va-80.html
- https://www.docsity.com/en/thermal-death-time-experiment-microbiology-lab-manual/455124/
Thermal death time, thermal death time pdf, how to calculate thermal death time, thermal death point of E coli, thermal death point of bacteria, TDT microbiology, thermal death point example, difference between thermal death point and thermal death time
FAQs
The lowest temperature at which all microorganisms perish after a 10-minute exposure is known as a microorganism’s thermal death point (TDP).
Yes, by using spectrophotometrically, cell counter, epifluorescent microscopy etc.
🔴 Would you like to attempt Labmonk Daily quiz? Click here
🔵 Check out Jobs & Exam Notices. Labmonk Notice Board
🔴 Labmonk Scholarships. Click here
🔵 Labmonk Blog. Click here
🔴 Do you need notes? Click here
Watch Career related videos on Youtube: Watch now !!


